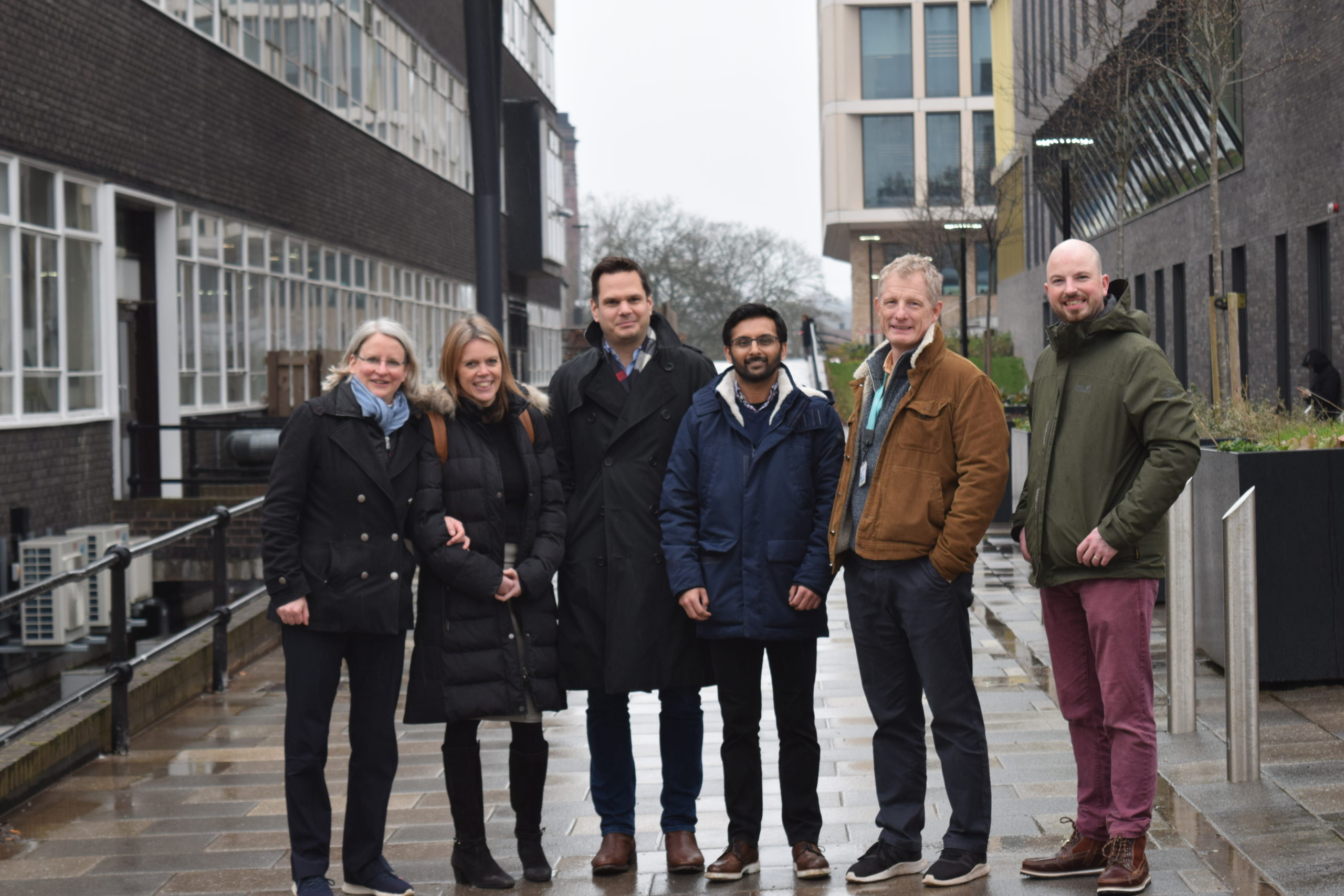
We are delighted to announce our decision to provide a grant to fund a research project concerning fusion-negative rhabdomyosarcoma (RMS). This project will commence on 1st March 2021 and will be led by Dr Susanne Gatz at the University of Birmingham. The team also comprises Professor Jo Morris, Professor Ferenc Mueller and Dr Joseph Wragg, and a PhD student will join the team in October 2021.
Fusion negative RMS accounts for about 75% of all newly diagnosed RMS and 50% of all relapses are fusion-negative. Importantly, RAS pathway gene mutations are present in ~ 50% of this fusion negative group and identifying new treatments for RMS with these changes could make a huge difference to RMS patients. This project aims to increase our understanding of RAS pathway alterations in RMS, focusing on DNA repair and replication stress. Research into normal cells and other cancers suggests that RAS pathway alterations change the way that cells deal with tasks like replicating their DNA and repairing defects in their DNA. The team hypothesizes that this change can be exploited in RMS cells with combination treatments including DNA repair inhibitor drugs already licensed or under study in clinical trials. It’s ultimate goal is to identify new and tailored treatments for this population of RMS patients that can feed into established academic clinical trials such as FaR-RMS, which is led by the Cancer Research Clinical Trials Unit (CRCTU) at the University of Birmingham.
An innovative Zebrafish larvae tumour xenograft model will be used for the in vivo drug screening. Zebrafish larvae have a number of attributes which make them uniquely amenable to cancer research. They are transparent which allows direct observation of tumour cell behaviour; they rapidly reproduce providing hundreds of fish larvae for injection with human 3D tumour models per day, making it a highly scalable platform for drug screening. There are additionally significant biological similarities in cancer signalling pathways between humans and fish. All these factors make this model a promising tool to help speed up the paediatric cancer drug discovery process.
Dr Susanne Gatz, Senior Clinical Lecturer in Paediatric Oncology commented “Around 60 children per year in the UK are diagnosed with rhabdomyosarcoma and for those presenting with metastatic or relapsed disease the prognosis is dismal. In most cases, there are no curative treatment options available on relapse and we want to change this. We can only make progress towards this by conducting these crucial research projects and securing grants from charities like Alice’s Arc and I am incredibly grateful for Alice’s Arc’s support of this important, innovative project.”
Sara and David Wakeling, founders of Alice’s Arc said “We believe this project will contribute to achieving our research priorities. Our goals are to invest in innovative research that can be translated to clinical trials creating more treatment options for children with relapsed disease and consequently improving survival rates for children with rhabdomyosarcoma. We look forward to working with the team at the University of Birmingham on this important piece of research.”