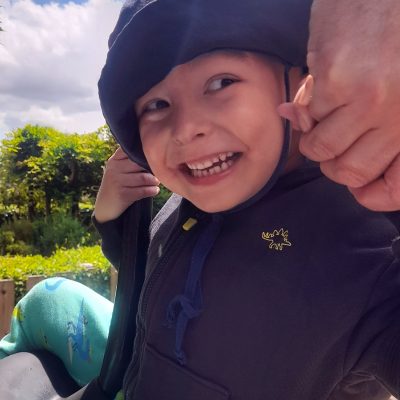
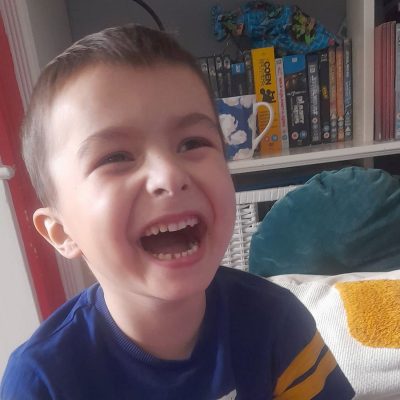
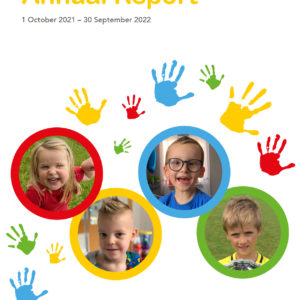
In the middle of August 2021, a few weeks before Elliott was to start school, he began to wake in the night with pain in his cheek. This was out of character, as he had always been a good sleeper. We took him to our GP hoping she could find a reason for this uncharacteristic night pain. We were told it was residual pain from a cold, and told to give him paracetamol, and ibuprofen, as needed. The pain continued and we took him back to the surgery where Elliott was seen by another GP who gave the same diagnosis and advice.
At the start of September, Elliott started school. We noticed his behaviour was out of character, and was less enthusiastic than we had expected, as he usually loved being with his peers. This was exacerbated by his sleepless nights. It didn’t feel right, and we took him to the dentist to see if his oral health was behind the pain, but nothing was observed.
The pain continued and we took him back to the GP on 20th September. A paediatric referral was made for him and we were told we would know the date in about a week, where we could then decide if we wanted to choose private consultation instead. The expectation we were given for this referred appointment was that he wouldn’t receive an ultrasound, as it was unlikely to pick up anything regarding soft tissue, and that he might require a CT scan and have to have a general anaesthetic. We were told that, after examining Elliott that day, there were no worrying signs of anything serious, and to continue to give him ibuprofen at night. Continuing to feel frustrated by Elliott’s discomfort we called the surgery one more time at the end of September to check if a date had been made for his referral, and were advised to wait for the paediatric referral, and to continue with paracetamol and ibuprofen.
On 30th of September, before we got the date for his paediatric appointment, which was eventually scheduled for November, his teacher called us from school, concerned with his behaviour and mood. We kept him off school the following day and called the surgery again. The GP we spoke to this time said that if we were concerned, we should take him to A&E. When he was examined at A&E, it was noticed that he had developed a swelling on the right side of his face that made his features non symmetrical, and he was admitted onto Lions ward at Royal Berkshire Hospital. He was put onto broad-spectrum antibiotics as a precaution. He was examined the next day by the ENT specialist, who was unable to find a cause for the swelling, and arranged for Elliott to be transferred to the Childrens Hospital at the John Radcliffe Hospital in Oxford. Once there he had a facial ultrasound, which showed a presence of concern, and prompted for Elliott to have an MRI scan under general anaesthetic. The results of this scan on Thursday 7th October, well over a month after we had first taken Elliott to the GP complaining of pain, were devastating. The scan showed a malignant mass in his right jaw with intra-cranial extension.
At that point, we both left work to be with him. He then had a biopsy under general anaesthetic to assess the tumour they had found. We were sent home with the expectation of a return to Oxford to discuss the findings of the biopsy. When we arrived for this appointment, we were told that Elliott had a malignant fast growing unresectable tumour which they would soon identify to enable treatment to begin. We crumbled in front of the medical professionals present. After we composed ourselves, we were taken to John Radcliffe’s paediatric oncology ward, Kamran’s ward, where we were introduced to the team of Drs, nurses, and consultants, who would be taking care of Elliott. They told us the biopsy showed that Elliott had Embryonal Rhabdomyosarcoma. Once we had the biopsy results, the pace of treatment and care moved into a different gear. Even though we were still in disbelief about our situation and overwhelmed by what was happening, for the first time in months we felt that Elliott was getting the care he needed.
We were shocked when we heard that day that Elliott needed to go under GA again to have a full body MRI scan, CT scan and bone marrow asparation for staging the cancer. He also needed to have a Hickman Line putting into his chest to make routine blood tests and medicines easier and less painful. More upsetting was that our bright boy of just 4 years knew exactly what was required of him, saying, ‘I don’t want them to put that in my chest’. After his line was fitted, Elliott began his first round of very high-risk intensive IVADo chemotherapy on Wednesday 20th October. It transpired from his scans and biopsies that he had Very high Risk Metastatic Embryonal Rhabdomyosarcoma.
The vomiting and loss of appetite the chemotherapy caused was hard to witness. It was so bad that Elliott was unable to keep down the nasal gastric tubes he needed to supplement his calorie and fluid intake to maintain a healthy weight. On this basis, it was arranged for him to have a gastro peg fitted into his stomach. This had complications including swelling that at one point enveloped the gastro peg. After returning to Kamrans to receive specialist care to resolve this, we began to see the benefits with him gaining weight again.
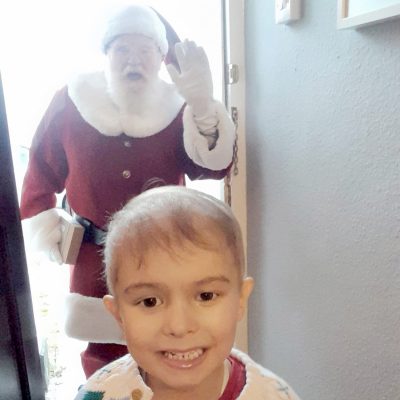
The weight loss, hair loss, and severe constipation that followed, made the lead up to Christmas challenging. The chemotherapy lowered Elliott’s immunity, making him neutropenic. We often had to shield so he didn’t catch covid and miss his next cycle of chemotherapy. When he frequently had a temperature, we had to visit the isolation rooms on Lion’s Ward at Royal Berks Hospital, where he would receive the antibiotics, blood transfusions, and platelet transfusions required to stabilise him. We were almost on the ward for Christmas Day. In addition to these complications, the swelling caused by the tumour had caused Elliott’s right eyelid to stay open slightly and dry out as he slept. This in turn caused him to develop a corneal stromal scar. Elliott would now require frequent eye ointment each day.
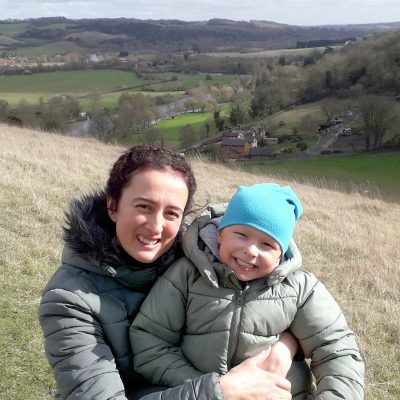
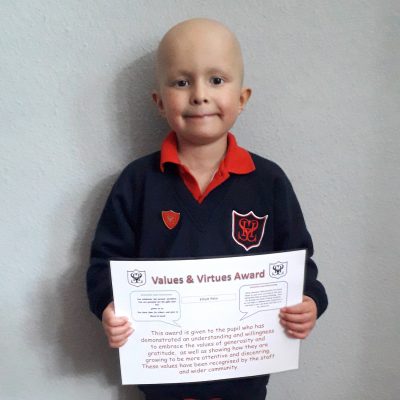
On Christmas Eve 2021 we were told that the chemotherapy had begun to shrink his tumour and metastases. With brilliant support from Kamran’s ward and the community teams, we got better at managing the side effects of his treatment, and were delighted to hear in March 2022 that his cancer had reduced significantly. The slivers remaining, however were unresectable, and were a reminder that he had yet to beat this cancer. The next option was to complete a 5 1/2 week course of radiotherapy at UCLH. We were also put onto the FaR-RMS trial, and randomised for the standard dose of radiation. It was decided by the proton panel that Elliott should receive photon, instead of proton beam treatment, as his cancer had metastasised at diagnosis. He began the radiotherapy in late May 2022. This was hard as we were away from home for 5 1/2 weeks. Because of his age he had to have GA for each daily dose of radiotherapy which meant being nil by mouth until 11am most days. After 3 weeks he began to get sores and feel lethargic from the treatment too. The radiotherapy also affected his ability to make tears in the right eye, so we had to escalate his eye ointment. Once the radiotherapy finished we began maintenance chemotherapy, to finish off the residual metastatic sites. When we returned home, Elliott, who had excellent virtual support from his teacher and educational support on the wards, was finally able to return to school. It was so good to see him back with his mates, doing what he should have been doing. One of the consequences of attending school was that he caught covid, and spent 3 weeks in isolation and prevented him being able to take some of his maintenance chemotherapy.
Elliott’s follow up scan after the radiotherapy on 19th August 2022 showed a thickening at the right side of the base of the skull. He had a follow up scan 4 weeks after this, which confirmed the swelling was a recurrance of his tumour, and not inflammation from the radiotherapy. We were devastated to hear this news, but were keen to pursue the second line VIT treatment available. This meant more hospital, more hair loss, and more reduced immunity. He was also prescribed new medicine for nerve pain and a preventative for epilepsy. After six weeks it became clear that this treatment was not working. With the rate at which the cancer had reoccurred, we were suddenly in a situation where we didn’t have time to effectively pursue alternative treatment. We now focussed our efforts on creating memories and life experiences, with palliative support from Kamran’s ward and Helen House and Alexander Devine hospices.
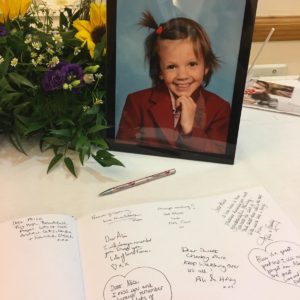
The symptom management support he received allowed him to fulfil his wish list. He was actively doing the things he loved until 30th November when he had a bad day with lots of sleep. After an unsettled night and seizure in the early hours of 1st December Elliott went to heaven at 11:15am later that morning at Helen House.