Maggie first experienced pain in her left hip after we got back from our holiday in France in April 2022. She also started having nose bleeds. We booked an appointment with the GP. Her doctor put it down to “growing pains” and she was referred for physiotherapy. She was prescribed pain relief, but nothing helped. At first, we thought she’d pulled her back by lifting her suitcase on holiday – her physio suspected a slipped disc. We did the exercises given, but at this point, she was struggling and in a lot of discomfort. After a few weeks, we phoned the GP and asked for another appointment.
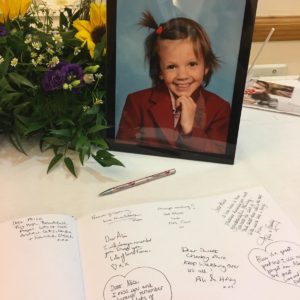
Maggie was having frequent nose bleeds and started to develop bruises. She was also complaining of tiredness and stomach discomfort, quickly feeling full whilst eating. It’s now the 20th of May – her 17th birthday. She continues to go to school but is feeling progressively more tired and has nose bleeds at least 2-3 times a day.
We saw the doctor on 25th May. At this point, I asked for a blood test because of her bruises and nosebleeds, no blood test had been requested up until this point, despite Maggie having several visits to her GP. The GP requested an MRI scan and blood test, although these appointments were still not immediate.
On 26th May, Maggie’s teacher rang us and asked if we could pick her up as she was not feeling very well. I phoned 111, and they advised me to bring her to A&E for a blood test. Maggie hesitated at first and told me that she just needed to sleep and rest. The A&E doctor commented to me that the blood test was deranged. He said that the blood test did not match how Maggie was at that time. Maggie was chatting and smiling at the doctor.
They advised Maggie to stay for a night to monitor her. We still didn’t have a diagnosis. She was admitted to Derby children’s hospital. Maggie was happy for me and her dad to go home and have a rest. She said she would message us if she needed us, and that she would be okay in the ward. I couldn’t sleep that night, so we returned to the hospital in the early hours of 27th May. We were told that Maggie had fainted at 2am. She continued to deteriorate that day; she was sick, her blood pressure was very low. Each time she tried to sit up or stand, she would faint. I spoke to the consultant and insisted that Maggie needed urgent attention. The doctor still didn’t not know what was happening to her, there was still no diagnosis.
That afternoon, the team decided to transfer here to the high-dependency unit in Derby; she was very poorly. At 1:30 am. on 28th May, she was blue-lighted to Nottingham intensive care unit. The oncology consultant on-call that evening gave us the consent form to sign, and she explained that they planned to give Maggie a high dose of dexamethasone and retinol acid chemotherapy. They thought that she had APML. We were told that she was very poorly, and they didn’t know if she would survive the night.
We were told that Maggie presented with disseminated intravascular coagulation, pleural infusion, fluid overload, and tumour lysis. Maggie continued to deteriorate; she had difficulty breathing; she was given oxygen through an assisted breathing machine. She also had a central line and nasogastric feeding tube fitted. We still don’t have a definitive diagnosis at this point. She had a bone marrow biopsy on 31st May.
On 1st June, we were told that the diagnosis was metastatic fusion-positive Alveolar Rhabdomyosarcoma. We have never heard of it. We were very shocked and confused about what the future held. On 2nd June 2022, she was given the first cycle of Ifosphamide, Vincristine, actinomycine D, Doxorubicin (IVAdo) treatment and was enrolled on the FaR-RMS study.
Maggie continued to make slow progress; her blood test results were gradually stabilising. The team decided to transfer Maggie to ward E39 – the children’s oncology ward in Nottingham. She had surgery to fit a port for chemotherapy administration. She became well enough to have tubes and cannulas removed. Maggie was allowed home on 17th June; she was very happy to be home. Her friends, who she missed very much, visited her.
Maggie finished twelve gruelling cycles of intensive chemotherapy, with numerous hospital admissions due to the side effects. Throughout the weeks of nausea, blood transfusions, hydration sessions, aches and pains, blood tests, scans, painful GCSF injections, and admissions due to infection, we never heard a single complaint from her. Maggie finished the last IVAdo cycle in the last week of December 2022.
Maggie had a PET scan post IVAdo treatment and was told that there was no evidence of disease, she then started maintenance chemo (Vinorelbine and Cyclophosphamide) in December 2022. Four weeks later she started to complain of headaches. A CT head scan in January 2023 confirmed that the cancer had spread to her brain. This was a shock after she had responded so well to the treatment.
At that point, we were told that she might have weeks or months to live. Maggie received six cycles of whole-brain radiotherapy. She was doing so well. The side effects were managed by steroids. We were told that further treatments were limited at this point. Maggie was a fighter, and always believed there were more options available to her. We researched and contacted leading hospitals around the world to see if we could try anything. We started incorporating a more holistic approach which focused on the metabolic processes of her cancer, guided privately by the Care Oncology Clinic. Maggie started the second line of Vincristine, Irinotecan, Temozolomide (VIT) treatment. She was very ill after the first cycle with nausea and vomiting. She was admitted several times because of the side effects.
In February 2023, we started fundraising to help grant Maggie’s wishes and to potentially fund treatments unavailable from the NHS. Maggie believed that if she couldn’t live longer, she would live deeper. We travelled to her favourite places in between her treatments in Paris, Italy, and the UK. Upon our return, Maggie’s treatment was changed due to the side effects. Maggie started having dizzy spells in early May. She had a CT head scan which appeared to show significant reduction of metastatic disease in the brain. She was prescribed motion sickness tablets, which helped at first.
Maggie started a new regime of chemotherapy on 22nd May 2023. She was given Intrathecal Topotecan but after the first treatment she suffered dizziness when she stood up and was sick. Her balance was also affected. She was given hydration; on the assumption that the dizziness could have been caused by dehydration. After a week Maggie had the second dose. The dizziness worsened and the effect on her balance became more noticeable. She was very ill. She was admitted and had a CT head scan, which at that time showed a reduction of cancer. Then, for the first time since diagnosis, Maggie had a seizure. She was given anti-epilepsy drugs and steroids.
At that point, we had a very difficult conversation with the medical team. Her oncologist thought that this could be a deterioration caused by her cancer. That was the first time we talked about moving her to a hospice. It was very difficult. We spoke to Maggie about the idea of moving to Rainbows hospice and potentially going home if she recovered. We decided as a family that the hospice was a good place for all of us, but she quickly deteriorated. After just over a week at Rainbows Maggie passed away on 20th June 2023.